Modern Abutment Design And Its Importance
By Nitzan Levy for MSDI Implants Academy | July 31, 2025
Let’s be clear – abutment design isn’t just about esthetics anymore.
It plays a direct role in soft tissue stability, bone preservation, and long-term implant success [1][2].
From concave profiles to anodized surfaces and custom CAD/CAM workflows, modern abutments are engineered with biology in mind.
Let’s break down what makes them different and why it matters.
What Makes an Abutment “Modern”?
Today’s abutments are all about precision, tissue preservation, and long-term performance. Here’s what sets them apart:
Anatomic and Concave Emergence Profiles
The emergence profile (the shape of the abutment as it exits the implant and passes through the soft tissue), has a major impact on healing and esthetics. Why they work better?
Mimic natural contours: They align better with the soft tissue and look more like a natural tooth [1][3].
Create a soft tissue chamber: The inward curve allows soft tissue to thicken and mature around the implant [1][3][5].
Help preserve bone: A thicker mucosal seal reduces crestal bone resorption over time [1][3][6].
Design with strength in mind: Even with a concave profile, mechanical stability must remain uncompromised [2].
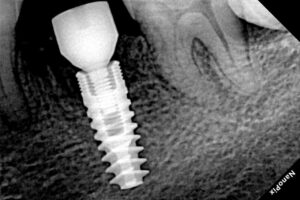
Secure Connections
A strong connection is key to preventing complications like screw loosening or microleakage. Modern designs like Internal Hex or Morse Taper offer a tighter seal, less movement under load, and better preservation of bone and soft tissue [2][5][6].
Materials that Work
Titanium: Still the gold standard – strong, biocompatible, and excellent for soft tissue attachment[1][2][7].
Zirconia: Matches the translucency of natural teeth – ideal for esthetic zones[1][2].
Polymers (PEEK, PMMA): Useful for temporary or chairside solutions. Good compatibility, but still evolving in long-term studies [1].
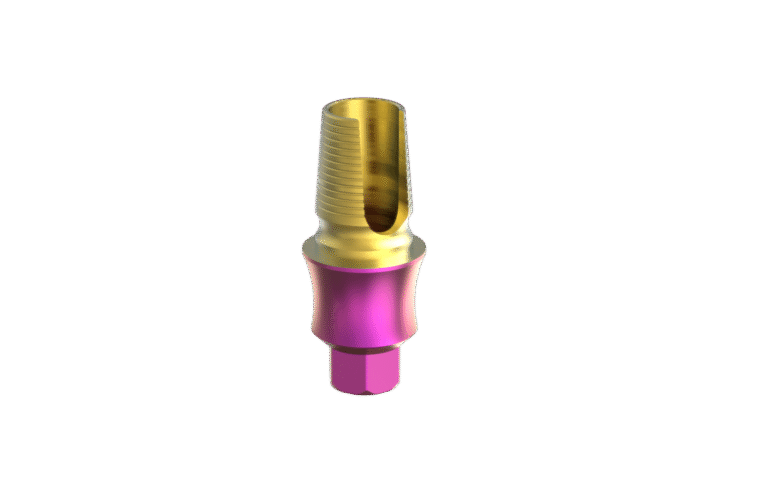
Surface Treatments & Anodization
Anodized titanium: Adds a thicker oxide layer and allows color options (like pink or gold) to reduce gray show-through under thin tissue. It improves soft tissue response, corrosion resistance, and biologic sealing[1].
Other surface mods: Sandblasting, acid-etching, and bioactive coatings also help reduce inflammation and support tissue health[1][2].
CAD/CAM Customization
Digital workflows allow for fully individualized abutments that fit perfectly and allow for a better soft tissue support, improved esthetics, fewer prosthetic complications, and more efficient lab-clinic communication [1][2]
Ti-base Abutments
What are Ti-bases?
Titanium bases (Ti-bases) are prefabricated titanium components that serve as the link between the implant and the final restoration. They offer a durable, biocompatible foundation for crowns or bridges fabricated using CAD/CAM technology and bonded extraorally.
Their standardized design ensures mechanical strength, precision fit, and long-term resistance to corrosion – all crucial for implant longevity and soft tissue health[8][9].
What makes a good Ti-bases?
Not all Ti-bases are created equal. Here’s what defines a high-quality one:
Accurate fit: Minimal microgaps mean fewer bacterial risks and better tissue preservation.
Mechanical strength: High fracture resistance ensures the abutment holds up under occlusal forces.
Digital compatibility: Designed to work seamlessly with CAD/CAM workflows for accurate restorations.
Strong bonding: Optimized for secure extraoral cementation using resin cements.
Soft tissue friendly: Biocompatibility supports epithelial adhesion and healthy soft tissue response.
Clinical data shows survival rates of 98.6% at 1 year, with performance on par with other abutment types[8][9][10].
Why Emergence Profile Still Matters on Ti-Bases
Even with a solid base, the emergence profile plays a critical biological role.
Choosing a concave emergence design helps to promote soft tissue thickening, encourage papillae formation, preserve marginal bone, and enable personalized restoration via CAD/CAM.
Simply put: Ti-bases give you strength. Anatomic profiles give you soft tissue stability. You need both.
What Is an Angled Screw Channel (ASC) Ti-Base?
Angled Screw Channel Ti-bases (Like the EleganTi™ by MSDI) are designed to allow the prosthetic screw to enter at an angle (typically up to 25°), rather than directly along the implant axis. They are usually used:
When implants are placed non-axially and straight screw access would compromise esthetics
To redirect the screw access away from visible facial or incisal surfaces
When esthetic zones or limited vertical space rule out straight access
Benefits of ASC Ti-Bases:
Improved esthetics – screw access is hidden, no visible metal
Maintains strength – similar fracture resistance to straight screw designs
Preserves retrievability – enables screw-retained prostheses in esthetic zones
Flexible protocols – suitable for immediate or delayed loading [11][12]
Why It All Matters: Clinical Outcomes
Protecting Soft and Hard Tissue
Studies show that emergence profile, connection stability, and material selection directly affect marginal bone levels and soft tissue integrity [1][3][6].
Better Esthetics
Using customized, anodized titanium abutments helps maintain the gingival margin and improves the overall esthetic outcome – especially in visible zones [1][2].
Fewer Mechanical Failures
Strong connections and proper material selection reduce the risk of screw loosening, fractures, or microleakage [2][5][6][3].
Lower Risk of Inflammation
Modern surface treatments improve epithelial attachment and reduce bacterial adhesion – critical for avoiding peri-implantitis and supporting long-term restoration success [1][2].
Clinical Recommendations
Here’s how to put this into practice:
Regularly use modern abutments with anatomic emergence profiles whenever possible [1][3].
Choose Titanium or Zirconia [1][2].
Prefer anodized abutments if possible to support soft tissue integration and reduce gray shine-through [1].
Embrace digital workflows to achieve precision and repeatability [1][2].
Select reliable secure connection types like internal hex or Morse Taper to preserve mechanical and biological integrity [2][5][6].
Final Thought
From connection geometry to emergence profile, material selection to surface treatments – every design decision matters.
Whether you’re choosing a custom abutment or planning a screw-retained zirconia crown on a Ti-base, the key is balancing mechanical strength with biologic integration.
Modern abutments, including ASC Ti-bases, give you tools to meet both demands. Use them wisely, and your restorations will last longer, look better, and keep your patients happier.
References
Chokaree P, et al. Biomaterials and Clinical Applications of Customized Healing Abutments for Dental Implants: A Narrative Review. Polymers. 2022. [PMC9781385]
Totou D, et al. Esthetic, mechanical, and biological outcomes of various materials for implant abutments: A systematic review. J Esthet Restor Dent. 2021. [PMC8423965]
Yağır MO, et al. Examination of Various Abutment Designs Behavior Regarding the Surrounding Bone Using 3D FEA. Nanomaterials. 2024.
Influence of Different Abutment Designs on the Biomechanical Behavior of One-Piece Zirconia Dental Implants: A 3D-FEA Study. Bohrium. 2024.
Romanos GE. The implant-abutment connection and its impact on prevention of bone loss: Literature review. Front Oral Maxillofac Med. 2023.
Schmidt AC, et al. Effect of Implant-Abutment Connection on Bone Level and Complications. 2024.
Ma M, et al. Mechanical properties and marginal fit of prefabricated vs. customized dental implant abutments. Clin Implant Dent Relat Res. 2022.
Chantler JGM, Evans CDJ, Zitzmann NU, Derksen W. Clinical performance of single implant prostheses restored using titanium base abutments: A systematic review and meta‐analysis. Clin Oral Impl Res. 2023. [PMID 37750524]
ITI Academy Clinical Consensus: Clinical performance of single implant prostheses restored using titanium base abutments. 2023.
Al-Thobity AM. Titanium Base Abutments in Implant Prosthodontics: A Literature Review. Polymers. 2021;13(4):498. [PMC8890922]
Mura P, Santoro M, et al. Angulated titanium bases screw channel abutments for single implant-supported crowns: A systematic review. J Prosthodont Res. 2025 Mar; [PMC9523696]
Schröder L, et al. Fracture resistance comparison between titanium and zirconia implant abutments with and without aging: Systematic review and meta-analysis. Materials. 2023.