Introduction
Ever wondered why some implant cases experience unexpected crestal bone loss – even when you’ve followed every guideline? You’re not alone. This issue is one of the most frequent challenges in implantology. The good news: multiple studies and expert protocols show how to significantly reduce it. Let’s explore proven strategies to protect your patients’ outcomes.
Why Crestal Bone Loss Happens
Crestal bone loss often stems from several risk factors:
Violation of the biologic width or biologic space
Overheating during osteotomy
Improper depth and angulation compromising primary stability
Implant-abutment interface designs
Thin mucosal biotypes around the implant
How to Minimize Bone Loss?
1. Maintain the Biologic Space
Biologic width, typically around 2–3 mm of surrounding soft tissue, dictates bone preservation. A study found that implants with an initial biologic width between 2.85 and 3.40 mm experienced the least bone loss (1). Those placed below crest level or in thin gingiva saw significantly more resorption (2, 3).
Ensure implants are placed at least 4 mm below the gingival margin and 2 mm from the vestibular plate to maintain this space.
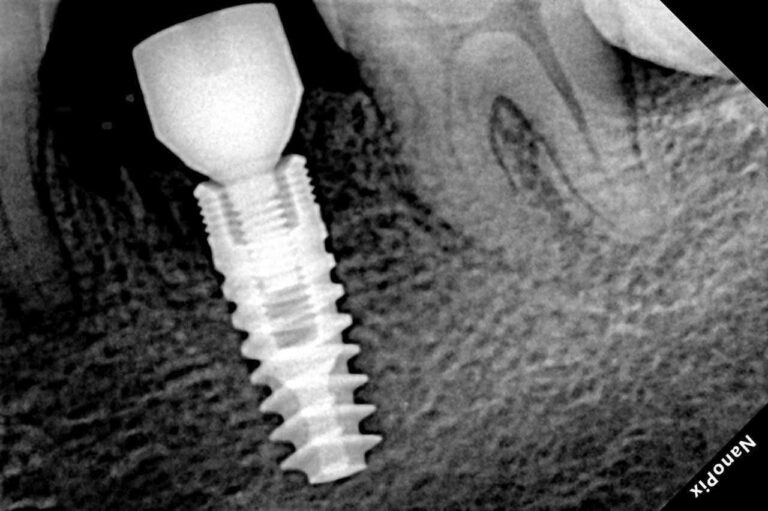
2. Optimal Implant Depth: Crestal vs. Subcrestal
Evidence shows:
A 5-year randomized trial comparing crestal vs. subcrestal placement showed slightly less bone loss with subcrestal placement (−0.80 mm vs −0.99 mm), though the difference wasn’t statistically significant (4).
A split-mouth RCT reported that subcrestal implants had similar long-term bone loss but moderately reduced exposure of rough surfaces over time (1).
Meta‑analyses concluded both crestal and subcrestal placements are effective long‑term, but subcrestal placement may better protect esthetics in thin tissue biotypes (5).
A retrospective study indicated optimal placement depth around 1–2 mm subcrestal resulted in minimal bone loss (6).
Consider placing implants 1-2 mm subcrestally, especially in thin tissue phenotypes or esthetic zones—to safeguard bone and soft tissues.
3. Respect Surgical Protocols
Adhere strictly to manufacturer’s drilling sequence – it’s tailored for optimal heat control.
Use sharp, fresh drills to reduce friction and prevent thermal trauma.
Ensure sufficient irrigation and avoid excess torque to prevent overheating, which can compromise osseointegration.
Studies show that sharp drills and correct irrigation result in significantly less crestal bone loss (6, 2).
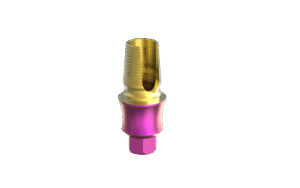
4. Micro-Design: Platform Switching & Connection
Platform switching –using a narrower abutment relative to the implant diameter, shifts the inflammatory zone inward, preserving crestal bone (7). Modern Concave / Anatomic designs do this very well.
Internal Conical connections offer better sealing and fewer microgaps, reducing microbial-driven bone loss. Evidence suggests subcrestal placement of conical implants is favorable (5).
5. Soft Tissue Management
Thin mucosa (< 2 mm) is associated with more bone remodeling. Ensuring at least 2 mm of mucosal thickness helps stabilize crestal bone (8).
In thin biotypes, consider soft tissue grafting or subcrestal placement to protect against recession and bone exposure.
Key Takeaways to minimize bone loss
Respect a 2.8–3.4 mm biologic width, staying 4 mm from gingival margin and at least 2 mm from vestibular plate
Favor 1-2 mm subcrestal implant placement, especially in thin tissue zones
Stick to sharp drills, adequate irrigation, correct angulation, and full protocol compliance
Use platform-switched, Anatomical abutments for improved bone preservation
Manage soft tissue biotype actively through grafting or strategic placement
Implementing these strategies can dramatically reduce early bone loss, improve esthetic outcomes, and protect implant longevity.
We’d love to hear about your results—share your cases with us!
References:
Dr. Rafa Vila Tello is a renowned implantologist, international lecturer, and Director of Clínica Dental Vila Tello in Valencia, Spain. He serves as a professor at the Instituto Valenciano de Investigaciones Odontológicas (IVIO) and is a co-founder of Dental Academia Digital. He’s also the key opinion leader for MSDI, Henry Schein and Dentsply Sirona, and a frequent speaker on guided surgery, immediate loading, and advanced implant protocols at major congresses across Europe and Latin America.
Long-term performance of implants placed at crestal vs. subcrestal position.
The influence of biological width violation on marginal bone resorption dynamics around two-stage dental implants with a moderately rough fixture neck: A prospective clinical and radiographic longitudinal study.
Influence of soft tissue thickness on marginal bone level around dental implants: A systematic review with meta-analysis and trial-sequential.
Impact of platform switching on marginal peri-implant bone-level changes. A systematic review and meta-analysis.
Radiographic comparisons of crestal bone levels around implants placed with low-speed drilling and standard drilling protocols: Preliminary results
Platform switching for marginal bone preservation around dental implants: a systematic review and meta-analysis.
The influence of soft tissue thickness on crestal bone changes around implants: a 1-year prospective controlled clinical trial.