Dental Implant Failures: Who’s to Blame? A Research-Based Analysis
Introduction
Ever had a patient walk back in with a failed implant and felt the urge to blame the implant brand? You’re not alone – it’s a common reaction. But while implant failures are statistically low, the reasons behind them are complex, and focusing solely on the implant often misses the bigger picture. This approach can stall professional growth, obscuring opportunities to refine technique, patient selection, and follow-up care.
In this article, we have relied solely on high-quality, contemporary peer-reviewed research to break down the real culprits behind implant failures and offer an evidence-backed view on who (or what) might actually be responsible.
Incidence of Implant Failures
Dental implants boast high long-term survival rates, with systematic reviews reporting survival rates of approximately 96.4% at 10 years (Howe et al., 2022). However, failures do occur and can be broadly categorized into:
Early Failures: Occur before functional loading, often due to poor osseointegration, surgical trauma, or contamination (Bosshardt et al., 2017).
Late Failures: Occur after functional loading, usually due to mechanical complications, infection, or peri-implantitis (Berglundh et al., 2018).
Understanding these failure types is crucial for identifying underlying causes and prevention strategies.
A recent survey conducted on LinkedIn by Mr. Nitzan Levy among dental professionals found that 53% blamed the dentist, 13% blamed the patient, 5% blamed the implant, and 28% attributed it to “bad luck” or unpredictable biological factors. This perception gap highlights the need for a scientific, evidence-based understanding of implant failure mechanisms.
Primary Factors Contributing to Implant Failures
The success or failure of dental implants is influenced by three primary risk categories: patient-related factors, surgical & prosthetic factors, and implant-specific factors.
A. Patient-Related Factors
Several patient-related factors play a crucial role in implant failures. Systemic health conditions such as diabetes, osteoporosis, and autoimmune disorders can significantly impact osseointegration. Poorly controlled diabetes, for example, increases implant failure risk due to impaired wound healing and reduced immune response (Lin et al., 2022). Similarly, osteoporosis can reduce primary stability and necessitate preoperative bone assessments (Stavropoulos et al., 2018). Certain medications, including corticosteroids and SSRIs, also negatively affect osseointegration (Dreyer et al., 2018).
Lifestyle factors further complicate implant success. Smoking has been widely documented as a major risk factor, with smokers experiencing significantly higher failure rates than non-smokers (Chambrone et al., 2020). The increased failure rate is linked to impaired healing, reduced vascularization, and a higher incidence of peri-implantitis (Levin & Schwartz-Arad, 2021). Additionally, a history of periodontal disease has been strongly associated with peri-implantitis and implant loss, underscoring the importance of pre-implant periodontal treatment and strict maintenance (Sousa et al., 2016).
Bone quality and quantity also play a significant role. The ITI Consensus Report confirms that low bone density is a major contributor to failure risks (Gallucci et al., 2018). Advances such as CBCT imaging and guided bone regeneration (GBR) have improved treatment planning in patients with compromised bone structure (Bornstein et al., 2017).
B. Surgical & Prosthetic Factors
Surgical precision is paramount to successful implant placement. Excessive heat generation during drilling, surgical trauma, and improper site preparation can lead to early implant failure by impairing osseointegration (Buser et al., 2017). To mitigate these risks, careful surgical planning, the use of appropriate drilling techniques, and guided surgery have been shown to improve placement accuracy and minimize trauma (Tahmaseb et al., 2018). Proper 3D implant positioning is essential to avoid mechanical complications and to ensure long-term prosthetic success (Buser et al., 2017).
Prosthetic design also influences implant longevity. Occlusal overload and poorly designed prostheses can lead to implant micromovement, resulting in bone loss and eventual failure (Gallucci et al., 2018). Ensuring a balanced occlusion and using appropriate loading protocols can help reduce mechanical stress on the implant.
C. Implant-Specific Factors
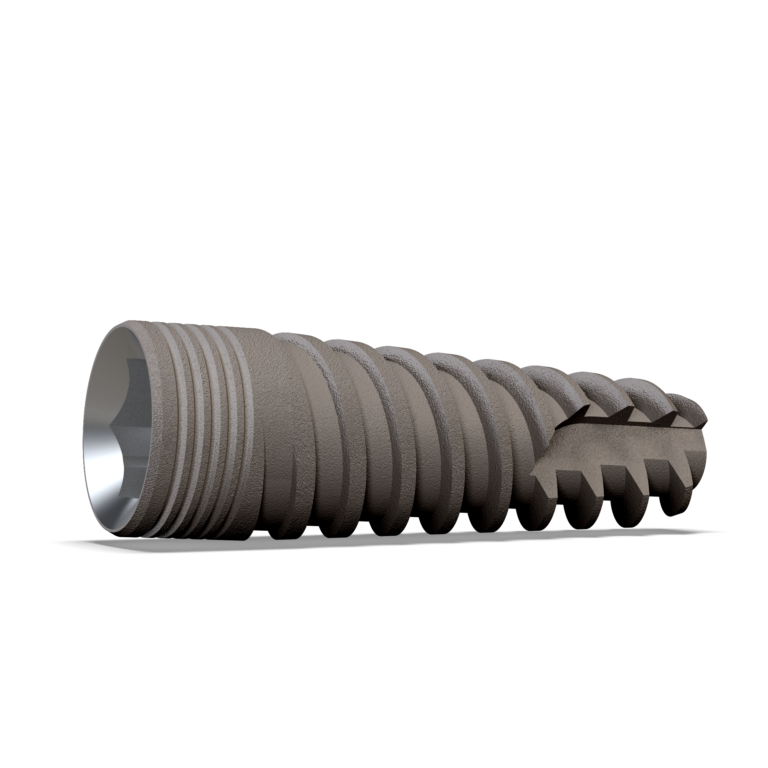
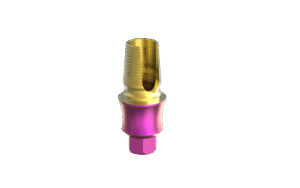
The choice of implant system and design plays a key role in osseointegration and long-term success. Moderately rough implant surfaces have been found to promote superior osseointegration compared to smoother alternatives (Doornewaard et al., 2019). Additionally, platform switching designs have been associated with reduced marginal bone loss and improved peri-implant soft tissue stability (Chrcanovic et al., 2018).
Despite debates over implant brand superiority, studies indicate no significant survival differences among major implant systems when proper surgical and prosthetic protocols are followed (Papaspyridakos et al., 2018). However, clinicians should remain cautious of counterfeit and low-quality implants, which may compromise outcomes.
Conclusion
So, who’s to blame for dental implant failures? The answer is not as straightforward as blaming a single entity. Implant success is a shared responsibility among the dentist, the patient, and the implant system itself.
While implant materials and designs have evolved significantly, no implant is immune to failure if surgical, prosthetic, or patient-related factors are not properly managed. Clinicians bear the responsibility of accurate diagnosis, proper treatment planning, and precision in surgical execution. Patients play a role in maintaining good oral hygiene, adhering to follow-up care, and managing systemic health conditions. Manufacturers must ensure high-quality implants, but even the best implant cannot overcome poor technique or inadequate post-operative care.
By proactively addressing these variables—through careful patient selection, precise surgery, and long-term maintenance—clinicians and patients together can significantly improve implant outcomes. Continued research and innovation in biomaterials, implant surfaces, and digital planning will further enhance implant longevity, making implant failures the exception rather than the rule.
References
Howe, M. S., et al. (2022). Journal of Dentistry, 122, 104152.
Bosshardt, D. D., et al. (2017). Periodontology 2000, 73(1), 7-26.
Berglundh, T., et al. (2018). Journal of Clinical Periodontology, 45(Suppl 20), S286-S291.
Lin, K. J., et al. (2022). Journal of Periodontology, 93(3), 327-339.
Stavropoulos, A., et al. (2018). Clinical Oral Implants Research, 29(1), 1-13.
Dreyer, C., et al. (2018). Quintessence International, 49(7), 563-572.
Chambrone, L., et al. (2020). Journal of Periodontology, 91(1), 9-18.
Levin, L., & Schwartz-Arad, D. (2021). Implant Dentistry, 30(5), 557-564.
Gallucci, G. O., et al. (2018). International Journal of Oral & Maxillofacial Implants, 33(Suppl 1), 116-134.
Bornstein, M. M., et al. (2017). International Journal of Oral & Maxillofacial Implants, 32(Suppl 1), s61-s77.
Sousa, V., et al. (2016). Clinical Oral Implants Research, 27(6), 652-666.
Buser, D., et al. (2017). International Journal of Oral & Maxillofacial Implants, 32(Suppl 1), 37-55.
Tahmaseb, A., et al. (2018). International Journal of Oral & Maxillofacial Implants, 33(3), 525-548.
Doornewaard, R., et al. (2019). Journal of Clinical Periodontology, 46(Suppl 21), 83-97.