Since their discovery few decades ago, dental implants have been widely used, mainly due to their aesthetic benefits. Because of their wide implementation, many scientific studies were done on various aspects of dental implants such as the effects of their shapes and surface modifications. This study will focus on the surface modification of dental implants,particularly the advantages of SLA surface modification over other surface modifications. It incorporates data from various scientific research including pre-clinical, clinical, multi center,and retrospective studies to show that SLA is reliable and has advantages over other types of surface modifications.
Introduction
In 1969, Branemark published a paper that described a process in which a titanium implant can be surgically inserted to stimulate tissue and bone growth around the implant1. The dental industry took a radical turn by this discovery of osseointegration, and many scientists began to research the different properties that affect bone-to-implant interface.
Although osseointegration is dependent on several factors, two main factors that affect osseointegration are geometry and surface topography. Tarly researchers focused on the shapes of the titanium implants and their effects on osseointegration. In the last decade, however, the focus of the dental industry shifted from the geometry topography to the surface topography because little research were done on this other important factor. As a result, many surface modifications including plasma-spayed, RBM (resorbable blast media), and SLA (sandblasted, large-grit, acid-etched) were developed. These surface modifications have shown to increase the success and survival rates of dental implants and to reduce the healing time after the surgical insertion of the implant2.
Many scientific research were done to compare the outcomes of different surface modifications. The most important data in these research are the survival and success rates. However, other important factors such as crestal bone loss, bone-to-implant contact, torque removal force, and long-term survival and success rates of these different surface modifications need to be compared as well3. This study will show that SLA is superior to other implant surface modifications in reference to these factors.
The SLA Process
The SLA surface modification consists of two steps: large-grit sandblasting and acid etching. These two steps complement each other to produce the optimal surface for osseointegration.
Large-grit Sandblasting with Al2O3
The first step of SLA is large-grit sandblasting The Advantages of SLA Surface Modification Abstract Since their discovery few decades ago, dental implants have been widely used, mainly due to their aesthetic benefits. Because of their wide implementation, many scientific studies were done on various aspects of dental implants such as the effects of their shapes and surface modifications. This study will focus on the surface modification of dental implants, particularly the advantages of SLA surface modification over other surface modifications. It incorporates data from various scientific research including pre-clinical, clinical, multicenter, and retrospective studies to show that SLA is reliable and has advantages over other types of surface modifications with Al2O3 which makes abrasions in the surface of the titanium implant4. The purpose of this step is to produce large depressions on the surfaces of implants which accelerates the process of osseointegration. A study by Buser et al. concluded that the roughness of the implant’s surface does have positive impact on the overall bone-to-implant interface5. Based on this study, large-grit sandblasting plays an important role in improving the overall success and survival rates of implants by creating roughness in their surfaces.
Acid-Etching
The second step of SLA is acid-etching. This process uses concentrated acids such as HCl and H2SO4 to remove residual particles from the sandblasting process. Also, acid-etching process generates small depressions in titanium implants. The combination of large depressions from the sandblasting and small depressions from acid-etching aids the process of osseointegration by producing the optimal surface roughness. This is proven by several studies which show that acid-etched surfaces increase the cell adhesion and the bone formation around titanium implants4.
Scientific Studies Regarding SLA
There are many scientific research that studied the effects of SLA on osseointegration. Some scientific studies focused solely on the survival rates and the success rates of SLA, while others focused on other factors of osseointegration such as removal torque force, pull-out strength, and bone structure. In all these criteria, SLA was shown to be effective and reliable to be used commercially.
Pre-Clinical Data
A study divided 12 minipigs into two experimental groups and a control group. Smooth-surfaced titanium implants with no surface modification were inserted into pigs in the control group, and titanium implants that were sandblasted or SLA surface treated were inserted into two experimental groups. Three implants were placed in each pig’s tibia, and an implant was placed in each pig’s vertebrae to start their experiment. The researchers used micro-CT analysis, mechanical testing, histological analysis, and statistical analysis to evaluate the results after 30 and 90 days.
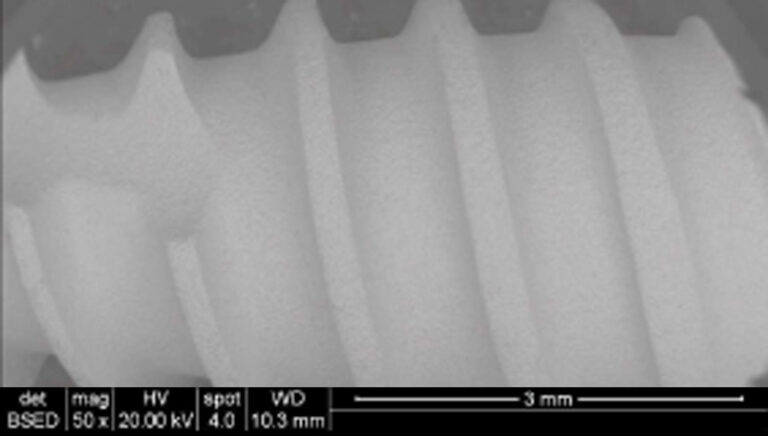
The results showed that implants with SLA surface were superior to implants with no surface modification and implants that were only sandblasted in all methods of analyses. The histological analysis showed that more bone structure and osteoblasts were formed along the SLA surfaced-treated Figure 1. MSDI implants with SLA surface modifications implants. Also, the mechanical test showed that the SLA surface treatment had the highest pull-out strength and removal torque force. Based on the data, the researchers concluded that the SLA surface treatment led to more stability and improved bone-to-implant interface than other groups3.
Clinical Data
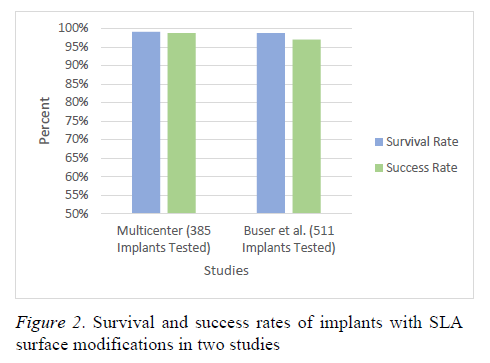
A multicenter study evaluated the survival rate and success rate of 385 implants with SLA surface in 120 patients. After 5 years, the survival rate and the success rate of these implants were 99.1% and 98.8%, respectively7. The difference between the survival rate and success rate is that the success rate is based on the number of implants which meet several criteria that define implants to be “successful” while survival rate is based on the number of implants that still in place regardless of their conditions.
A study by Buser et al. examined 303 patients who had 511 implants with SLA surface treatment from May 1997 to January 2001. Clinical data showed that these implants had a survival rate of 98.8% and a success rate of 97.0% after 10 years from the their insertion6. The results of this study show that SLA surface treatment is reliable years after surgical insertion (Figure 2).
Comparison of SLA with Other Surface Treatments
In this section, the scientific data of SLA and different surface treatments will be compared. Important aspects of dental implants such as survival rate, success rate, and crestal bone loss will be discussed.
Plasma-Sprayed Treatment vs. SLA
Plasma-sprayed treatment coats the implant surface with deposits. The most commonly used types are titanium-sprayed treatment (TPS) and hydroxyapatite-sprayed treatment (HA). The coating from plasma-sprayed treatment increases the surface area of the implant surface which encourages osseointegration.
One of the fundamental differences between this treatment and SLA is the method of generating roughness. Plasma-sprayed treatment is an additive surface treatment that incorporates deposits on the implant surface, while SLA is a type of subtractive surface treatment that bombards the implant surface with Al2O34.
Clinical Data
Studies have shown that the TPS and HA are effective in the short term but ineffective in the long term. The HA had a high failure rate in the long term partially due to the delamination of the HA layer.
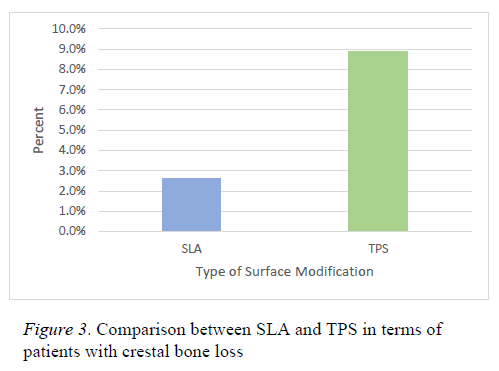
A retrospective study evaluated the survival rate and the crestal bone loss of SLA and TPS implants. From April 1994 to December 2005, 342 patients had 533 SLA and 303 TPS implants. The data from this study showed that SLA implants had a survival rate and a success rate of 97.4% and 96.1% respectively. The TPS implants had a survival rate and a success rate of 95% and 93.4%. Also, 2.6% and 8.9% of SLA and TPS patients respectively experienced crestal bone loss (Figure 3). This study showed that there were large differences in survival rate, success rate, and crestal bone loss between SLA and TPS.
The plasma-sprayed treatment such as HA and TPS was shown to be inferior to SLA in many different criteria. Plasma-sprayed treatment may be effective in the short term but proved to be unreliable for long-term use.
RBM vs SLA
Resorbable Blast Media (RBM) is a commonly used implant surface treatment which incorporates subtractive method similar to SLA. Although there are other differences between RBM and SLA, the main differences are that RBM uses calcium phosphate instead of aluminum oxide and that RBM does not use acid-etching process10. Compared to SLA-treated implants, implants that are treated with RBM method has a much rougher surface. Some studies have concluded that an excessively rough surface (>2 micron) has negative effects on osseointegration11.
Pre-Clinical Data
A study was done on the removal torque strength of implants with four different surface treatments. In this study, implants with RBM surface had the lowest removal torque while implants with SLA surface had the highest removal torque after 8 weeks. The fact that implants with SLA surface had higher removal torque than implants with RBM surface shows that SLA is superior to RBM in terms of osseointegration.
Clinical Data
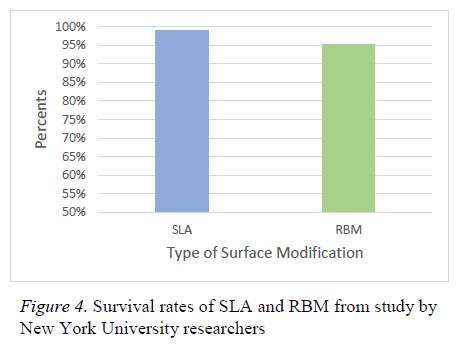
A research group led by researchers at New York University studied the survival rates of implants with SLA and RBM surfaces. 280 implants were placed in anterior maxilla, posterior maxilla, anterior mandible, and posterior mandible. This study determined that the survival rates of implants with SLA and RBM surfaces were 99.1% and 95.2% respectively10 (Figure 4).
The data from these studies show that SLA is superior to RBM in terms of removal torque and survival rates. One main reason for the differences is that implants with RBM surface is much rougher than those with SLA surface.
Conclusion
This study showed through the data from various studies that SLA is superior to other forms of surface modifications. Although the superiority of one surface modification over others are widely debated in both academia and in the industry, it should be noted that the differences among the surface modifications are not significant as concluded in a study14. All MSDI implants are treated by SLA surface modification; therefore, these implants are superior, or at least comparable to other major implant companies that utilize the same or other surface modifications.
References
1Brånemark PI, Adell R, Breine U, Hansson BO, Lindström J, Ohlsson A. Intra-osseous anchorage of dental prostheses. I. Experimental studies. Scand J Plast Reconstr Surg. 1969;3(2):81-100.
2Cochran DL, Buser D, Ten bruggenkate CM, et al. The use of reduced healing times on ITI implants with a sandblasted and acid-etched (SLA) surface: early results from clinical trials on ITI SLA implants. Clin Oral Implants Res. 2002;13(2):144-53.
3Lin TH, Hu HT, Wang HC, Wu MC, Wu SW, Yeh ML. Evaluation of osseous integration of titanium orthopedic screws with novel SLA treatment in porcine model. PLoS ONE. 2017;12(11):e0188364.
4Jemat A, Ghazali MJ, Razali M, Otsuka Y. Surface Modifications and Their Effects on Titanium Dental Implants. Biomed Res Int. 2015;2015:791725.
5Buser D, Schenk RK, Steinemann S, Fiorellini JP, Fox CH, Stich H. Influence of surface characteristics on bone integration of titanium implants. A histomorphometric study in miniature pigs. J Biomed Mater Res. 1991;25(7):889-902.
6Buser D, Janner SF, Wittneben JG, Brägger U, Ramseier CA, Salvi GE. 10-year survival and success rates of 511 titanium implants with a sandblasted and acid-etched surface: a retrospective study in 303 partially edentulous patients. Clin Implant Dent Relat Res. 2012;14(6):839-51.
7Cochran DL, Jackson JM, Bernard JP, et al. A 5-year prospective multicenter study of early loaded titanium implants with a sandblasted and acid-etched surface. Int J Oral Maxillofac Implants. 2011;26(6):1324-32.
8Esposito M, Hirsch JM, Lekholm U, Thomsen P. Failure patterns of four osseointegrated oral implant systems. J Mater Sci Mater Med. 1997;8(12):843-7. 9Arlin ML. Survival and success of sandblasted, large-grit, acid-etched and titanium plasma-sprayed implants: a retrospective study. J Can Dent Assoc. 2007;73(9):821.
10Ahmed E, Lee DH, Wang CW, Choon CH. Survival rate of RBM surface versus SLA surface in geometrically identical implant design. Jour Oral Bio. 2014
11Wennerberg A, Albrektsson T. Effects of titanium surface topography on bone integration: a systematic review. Clin Oral Implants Res. 2009;20 Suppl 4:172-84.
12Larsson C, Thomsen P, Aronsson BO, et al. Bone response to surface-modified titanium implants: studies on the early tissue response to machined and electropolished implants with different oxide thicknesses. Biomaterials. 1996;17(6):605-16.
13Ferguson SJ, Langhoff JD, Voelter K, et al. Biomechanical comparison of different surface modifications for dental implants. Int J Oral Maxillofac Implants. 2008;23(6):1037-46.
To view more studies click here